bowel management program


bowel management program
Dayton Children’s Hospital offers a multidisciplinary bowel management program designed for children dealing with refractory constipation or encopresis.
The multidisciplinary bowel management program at Dayton Children’s Hospital is for children who have refractory constipation or encopresis.
Refractory constipation is when a child is not able to poop regularly even after completing clean outs and taking laxatives (medication to help a person poop).
Encopresis is when a child leaks poop accidentally. These accidents usually happen due to the buildup of poop that is more difficult to pass with looser poop leaking around it. As the buildup of poop stretches the colon, the nerves have trouble telling the brain it’s time to poop. Accidents can be very embarrassing for your child, leading to denial and hiding soiled underpants.
If your child is referred to the bowel management program, they will see multiple health care providers in a single location to address all aspects of care for refractory constipation and encopresis.
what your poo is telling you
Many children have constipation at one time or another. Come along with Sarah as she explains the signs of constipation and what you can do if you’re experiencing similar symptoms.
who can benefit from the bowel management program?
- Children greater than 4 years of age
- Has constipation and encopresis for greater than 6 months
- Failed conservative management
- Completed more than two home bowel clean outs AND continuing maintenance bowel regimen following clean out without improvement in symptoms.
- Completed more than one inpatient clean out AND continuing maintenance bowel regimen following without improvement in symptoms.
- No additional contributing GI specific health issues (for example spinal cord abnormalities, anorectal malformations or Hirschsprung disease).
how long does the bowel management program last?
The program is tailored to an individual patient’s needs. While some patients may participate in the program for 12 months, others may experience a different timeline based on their needs.
- A video visit follow-up at 6 weeks (optional)
- Multidisciplinary visits in the office at 3, 6, 9 and 12 months
Families should plan 1.5 to 2 hours for each visit (except for the virtual follow-up at 6 weeks).
what testing may be considered while in the program?
- Screening labs (consideration of underlying medical conditions, if not already done)
- Abdominal X-rays (picture of abdomen to evaluate stool burden)
- Water soluble contrast enema (enema given by radiology staff filled with water soluble contrast material which enters the colon and highlights the anatomy of the colon)
- Anorectal manometry testing (assessment of pressure and sensations in the rectum)
what are management options considered while in the program?
Your child may need to do home bowel clean outs and maintenance laxative regimens using rectal therapy (suppository or enema), stool softeners and stimulant laxatives.
Your child may need additional or ongoing visits with physical therapy for pelvic floor training and/or with psychology for behavioral health management.
We will provide necessary school resources (i.e., 504 plan information, notes for bathroom privileges, etc).
Certain dietary modifications may be recommended.
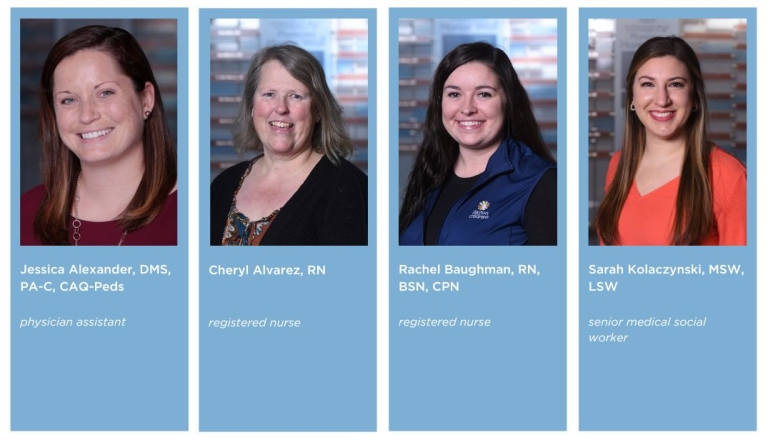
what will my child’s care team look like?
Your child will be seen by a physician assistant (medical provider), psychologist, social worker, dietitian, physical therapist and a nurse.


here when you need us
Whether you’re looking for the right provider, ready to make an appointment, or need care right now—we’re here to help you take the next step with confidence.
